
Summary of Benefits Coverage guidelines released: Another tool for benefits communication
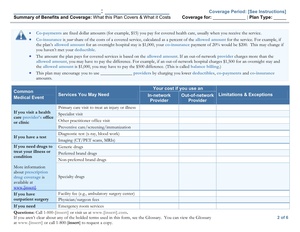 A couple of weeks ago, the Department of Labor (DOL) released its final regulations and guidelines for the Summary of Benefits Coverage (SBC), which provides people a standard template to compare the provisions of employer plans as well as those on the individual market. Well, it’s about time! While it lacks in certain areas, it goes a long way in explaining and clarifying what health care coverage means so that people can make informed decisions. We’re all for that!
A couple of weeks ago, the Department of Labor (DOL) released its final regulations and guidelines for the Summary of Benefits Coverage (SBC), which provides people a standard template to compare the provisions of employer plans as well as those on the individual market. Well, it’s about time! While it lacks in certain areas, it goes a long way in explaining and clarifying what health care coverage means so that people can make informed decisions. We’re all for that!
Here are some of the key highlights:
Implementation
The final regulations delay implementation by six months to give employers and insurers more time to comply. Instead of March 23, 2012, the regulations become effective September 23, 2012. What that means for you: Assuming you offer electronic enrollment, employees will need to receive an SBC for all health plan options they’re eligible for by the first day of your open enrollment period. For plans with a January 1 effective date and an open enrollment period of October 15–November 15, you need to be sure that eligible participants have an SBC in hand by October 15. For those with spring or early summer plan-year effective dates, the same principles would apply, but you’re lucky to have more time to figure everything out.
Don’t get too used to them. These SBC templates apply only for the first year of the mandate. The DOL will release updated guidelines for 2014 that could include big changes.
Coverage examples
One of the key features is its “coverage examples,” which are being compared to nutrition facts labels on packaged foods. As EBN put it, “The coverage examples will illustrate sample medical situations and describe how much coverage the plan would provide in an event such as having a baby or managing Type II diabetes. These examples will help consumers understand and compare what they would have to pay under each plan they are considering.” The costs illustrated in these examples will be driven by the clinical guidelines maintained by the non-governmental Institutes of Medicine.
Delivery and appearance
Employers can deliver the SBC as a stand-alone document or in combination with other summary materials (for example, a summary plan description), as long as the SBC information is intact and prominently displayed at the beginning of the materials (such as immediately after the Table of Contents in a summary plan description). Given the timing, there’s a great opportunity to use these tools as part of your enrollment campaign.
They can deliver the document in electronic format but must follow the same safe harbor rules that govern other ERISA disclosures. The final regulations reference the recent Request for Information by the DOL as they contemplate possible changes in how legal notices can be electronically delivered. We’ll be watching closely for those developments.
The SBC can be in color or grayscale. The SBC cannot exceed four double-sided pages in length and must not include print smaller than 12-point font.
Language
The DOL will provide translated versions of the template in Spanish, Tagalog, Chinese, and Navajo—255 counties have populations where at least 10 percent are literate only in another language. Five states contain the majority of these counties: Alaska, Arizona, California, New Mexico, and Utah.
The glossary
The uniform glossary, which must be referenced in the SBC, explains terms commonly used in health insurance coverage, such as “deductible” and “co-payment.” Some definitions, such as “out-of-pocket limit” will need clarification, however. See below. The glossary’s definitions cannot be altered.
The fine print
An interesting nuance—you and your insurance partners are both legally bound to comply with these regulations. The final regulations assume that to avoid wasted effort and resources, you will sort out who will be the responsible party. Unless you plan to engage a new insurance partner for 2013, you will likely need to deal with a contract amendment.
Like other legally required notices, there are fines for “willfully” not providing these documents to plan participants.
Integrating the new requirements
You’ll probably run into several challenges—how to integrate these into your communication campaign, how much help you can expect from your carriers, deciding whether electronic delivery can work at your company, the big changes to the SBC planned for 2014 and others we haven’t even thought about!
For companies who already have robust education about their health plans, this new requirement will feel redundant and unnecessary. But the SBC is offering a chance for all Americans to make apples-to-apples comparisons between their health plan options—whether that’s comparing the multiple options you provide them or contrasting them with options available to them through a spouse or domestic partner’s plan or, starting in 2014, something on the individual market.
And, remember, these won’t replace the need to continue to educate people on their health care plans through effective communication. That’s where your benefits website, social media and all your other communication channels come in.
Any new tool you can add, such as the SBCs, that can help employees understand and appreciate their benefits will ultimately help you, the employer. Year after year, MetLife’s annual Employee Benefits Trends study shows that “employees who are satisfied with benefits are nearly three times as likely to express a strong sense of loyalty to their employers.” That’s good for everyone.
Follow-up: Standard definition to out-of-pocket limit not quite there yet
We want to thank everyone who acted on our call to send an email to the DOL requesting a standard definition to the out-of-pocket limit. Of the 322 comments submitted to the DOL about the SBC, 26 of them, or 8 percent, submitted our one-line wording. The out-of-pocket limit definition is still not perfect, but we know our voices were heard, and the issue is worth continuing to follow.
Work with Us
We partner with organizations that value their people first. Let’s talk.

Jennifer Benz, SVP Communications Leader, has been on the leading edge of employee benefits for more than 20 years and is an influential voice in the employee benefits industry.
