
Communicating Benefit Plan Changes
Since the early 1950s, a large multiemployer health and welfare fund has provided members with generous benefit plans, even in challenging times. But as medical and prescription drug costs have continued to climb for their plan, the Board of Trustees recognized they’d need to make significant changes—or the fund’s financial future would be at risk.

A Strategy of Transparency
Like many health and welfare funds in similar circumstances, our client needed to update its plans and its member expectations. In order to protect the long-term viability of the fund and also become compliant with new regulations, including ACA, the plan’s Board of Trustees recognized they’d need to make changes to provide valuable benefits while also securing the fund’s financial future.
The Trustees wanted to help plan participants use their benefits more efficiently, so members and their families would receive the right care, at the right cost, in the right setting. Participants needed to understand where to go for care when they were ill or injured—their doctor, urgent care center, or emergency room.
To help participants use their benefits more efficiently, the Trustees determined a smarter plan design would achieve these goals. Eliminating some benefits, such as out-of-network provider coverage, except for emergency benefits, would drive participants to seek preferred providers for care. The new plan design would also improve other benefits and offer new programs. By implementing these modifications, the fund could continue to provide a robust benefits plan and stabilize costs.
Still, for participants accustomed to generous health and welfare benefits, both Trustees and the fund administrator anticipated that certain changes would be a tough sell. So, we helped them approach the problem head on by applying our expertise in change management, benefits communications, and consumer marketing. We created a communication plan that delivered both good and bad news in a clear, concise way, and rolled out a campaign showcasing a new brand and new benefits, all with a strategy of transparency.
Your Attention, Please!
The fund needed to communicate a lot of complex plan adjustments to stakeholders—participants, dependents, employers, and union representatives. Messages would need to help participants understand how the changes would affect them, what actions they needed to take, and why change was necessary.
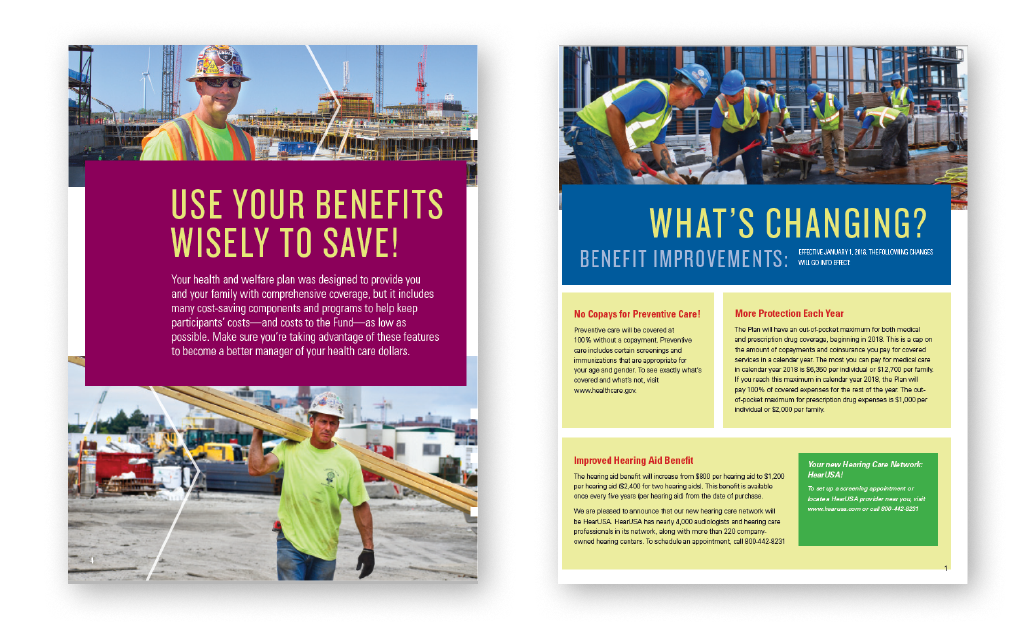
Based on their experience sending previous communications, the fund knew that participants tended to ignore mail from their insurance providers, but messages sent by the fund were read. To grab participants’ attention, we created a new brand for the fund and used photos of actual members on the job. This ensured the campaign would be noticed and that participants would pay attention to each communication. At the same time, participants would begin to associate the new brand with receiving important information from the fund.
To address the Trustees’ concern about how participants would react to the revisions, messages were rolled out slowly via multiple channels. PowerPoint presentations in English and Spanish were created for union meetings. Fund representatives followed the carefully scripted presentations to walk participants through the plan changes. Participants also received bilingual takeaway materials to share with family members—an overview letter and quick reference guide highlighting the plan changes.
The Award-Winning Result
While Trustees initially received some negative feedback and pushback to the changes, the campaign helped participants and union representatives understand, and ultimately accept, what was changing and why. Plus, by arming representatives with the rationale behind the changes, those reps were able to answer members’ questions and proactively support them while they learned about the differences in their benefits.
By getting ahead of the change and communicating with members early, we helped our client build trust with its participants and avoid misinformation and rumors from circulating. Trustees and the fund administrator ultimately received high praise about the benefit plan changes from participants.
Additionally, the campaign won a Gold Hermes Creative Award, the highest honor bestowed on the creators of communications campaigns who bring their ideas to life through traditional and digital platforms. A feather in the cap of this successful campaign rollout.
See More Client Stories

Expertise in change-management communication helps benefit leaders position plan changes to drive desired employee actions and achieve results.

A top financial services company leaps ahead with a global flexible time-off program.

NVIDIA takes a bold approach to promote new suite of benefits that targets Millennials in an epic enrollment campaign with epic results.
